Corporate Presentation SEPTEMBER 2022 Exhibit 99.1
Disclaimer The following presentation, including any printed or electronic copy of these slides, the talks given by the presenters, the information communicated during any delivery of the presentation and any question and answer session and any document or material distributed at or in connection with the presentation (collectively, the “Presentation”) has been prepared by Cabaletta Bio, Inc. (“we,” “us,” “our,” “Cabaletta” or the “Company”) and is made for informational purposes only. This Presentation does not purport to be a prospectus, to be complete or to contain all of the information you may desire. Statements contained herein are made as of the date of this Presentation unless stated otherwise, and this Presentation shall not under any circumstances create an implication that the information contained herein is correct as of any time after such date or that information will be updated or revised to reflect information that subsequently becomes available or changes occurring after the date hereof. This Presentation may contain “forward-looking statements” within the meaning of the Private Securities Litigation Reform Act of 1995 relating to our business, operations, and financial conditions, and include, but are not limited to, express or implied statements regarding our current beliefs, expectations and assumptions regarding: our business, future plans and strategies for our CAAR T technology and CABA™ platform; the progress and results of our DesCAARTes™ Phase 1 trial, including the significance and impact around the clinical and translational data updates from cohorts A1 through A4 of our DesCAARTes™ Phase 1 trial; the significance and impact around the 28-day safety for cohort A5 and clinical and translational data for cohort A4 at the 31st European Association of Dermatology and Venereology Congress; the therapeutic potential and clinical benefits of our product candidates; the expectation that Cabaletta Bio may improve outcomes for patients suffering from mucosal pemphigus vulgaris; our ability to escalate dosing as high as 10 to 15 billion cells in cohort A6m, initiate dosing in a combination cohort or otherwise; Cabaletta’s plans to implement a pre-treatment regimen and the potential ability to enhance in vivo DSG3-CAART exposure; our ability to advance dose escalation in the DesCAARTes™ Phase 1 trial at the current dose ranges for the current cohorts and any projected potential dose ranges for future cohorts, and to optimize our targeted cell therapy; our ability to evaluate, and the potential significance of, the relationship between DSG3-CAART persistence and potential clinical responses in patients with mPV; our ability to safely retreat additional patients and whether we will continue to observe a lack of immune-mediated clearance of DSG3-CAART cells after retreatment and repeat dosing of patients; our ability to successfully complete our preclinical and clinical studies for our product candidates, including our ongoing Phase 1 DesCAARTes™ trial, our planned clinical trial of MuSK-CAART, including our ability to enroll the requisite number of patients, dose each dosing cohort in the intended manner, and progress the trial; the ability of MuSK-CAART to target B cells that differentiate into antibody secreting cells, which produce autoantibodies against muscle-specific kinase; our ability to obtain and maintain regulatory approval of our product candidates, including our expectations regarding the intended incentives conferred by and ability to retain Orphan Drug Designation and Fast Track Designation for DSG3-CAART for the treatment of pemphigus vulgaris and Fast Track Designation for MuSK-CAART to improve activities of daily living and muscle strength in patients with MuSK antibody-positive myasthenia gravis; the further expansion and development of our modular CABA™ platform across a range of autoimmune diseases; our ability to contract with third-party suppliers and manufacturers, implement an enhanced manufacturing process and further develop our internal manufacturing strategy, capabilities and facilities; our potential commercial opportunities, including value and addressable market, for our product candidates; our expectations regarding our use of capital and other financial results; and our ability to fund operations through the first quarter of 2024. Words such as, but not limited to, “look forward to,” “believe,” “expect,” “anticipate,” “estimate,” “intend,” “plan,” “would,” “should” and “could,” and similar expressions or words, identify forward-looking statements. Various risks, uncertainties and assumptions could cause actual results to differ materially from those anticipated or implied in our forward-looking statements. Such risks and uncertainties include, but are not limited to, risks related to the success, cost, and timing of our product candidate development activities and preclinical studies and clinical trials, risks related to our ability to demonstrate sufficient evidence of safety, efficacy and tolerability in our preclinical studies and clinical trials of DSG3-CAART and MuSK-CAART, Cabaletta's plans to evaluate additional cohorts in the DesCAARTes™ trial, including a cohort implementing a pre-treatment regimen, the risk that signs of biologic activity or persistence may not inform long-term results, the risk that persistence observed with effective CART-19 oncology studies in combination with lymphodepletion is not indicative of, or applicable to, clinical responses in patients with mPV; risks related to clinical trial site activation or enrollment rates that are lower than expected, our ability to protect and maintain our intellectual property position, risks related to our relationship with third parties, uncertainties related to regulatory agencies’ evaluation of regulatory filings and other information related to our product candidates, our ability to retain and recognize the intended incentives conferred by any Orphan Drug Designation and Fast Track Designations, the risk that any one or more of our product candidates will not be successfully developed and commercialized, the risk that the results of preclinical studies or clinical studies will not be predictive of future results in connection with future studies, the impact of COVID-19 on the timing, progress, interpretability of data, and results of ongoing or planned clinical trials and risks relating to as a result of extraordinary events or circumstances such as the COVID-19 pandemic, and any business interruptions to our operations or to those of our clinical sites, manufacturers, suppliers, or other vendors resulting from the COVID-19 pandemic or similar public health crisis. New risks and uncertainties may emerge from time to time, and it is not possible to predict all risks and uncertainties. Except as required by applicable law, we do not plan to publicly update or revise any forward-looking statements contained herein, whether as a result of any new information, future events, changed circumstances or otherwise. Although we believe the expectations reflected in such forward-looking statements are reasonable, we can give no assurance that such expectations will prove to be correct. Accordingly, you are cautioned not to place undue reliance on these forward-looking statements. No representations or warranties (expressed or implied) are made about the accuracy of any such forward-looking statements. For a discussion of these and other risks and uncertainties, and other important factors, any of which could cause our actual results to differ materially from those contained in the forward-looking statements, see the section entitled "Risk Factors" in our most recent annual report on Form 10-K, as well as discussions of potential risks, uncertainties, and other important factors in our other filings with the Securities and Exchange Commission. Certain information contained in this Presentation relates to or is based on studies, publications, surveys and other data obtained from third-party sources and the Company’s own internal estimates and research. While the Company believes these third-party sources to be reliable as of the date of this Presentation, it has not independently verified, and makes no representation as to the adequacy, fairness, accuracy or completeness of, any information obtained from third-party sources. The Company is the owner of various trademarks, trade names and service marks. Certain other trademarks, trade names and service marks appearing in this Presentation are the property of third parties. Solely for convenience, the trademarks and trade names in this Presentation are referred to without the ® and TM symbols, but such references should not be construed as any indicator that their respective owners will not assert, to the fullest extent under applicable law, their rights thereto.
Develop and launch the first curative targeted cellular therapies for patients with autoimmune diseases
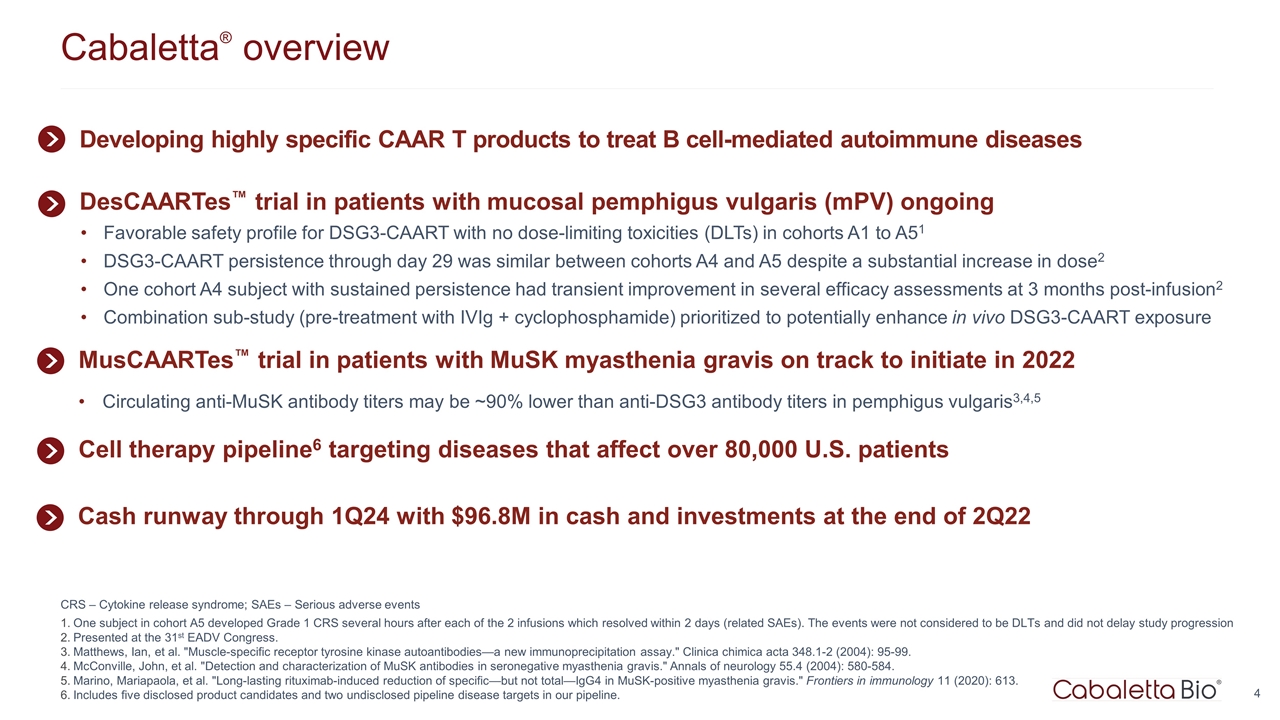
Cabaletta® overview CRS – Cytokine release syndrome; SAEs – Serious adverse events One subject in cohort A5 developed Grade 1 CRS several hours after each of the 2 infusions which resolved within 2 days (related SAEs). The events were not considered to be DLTs and did not delay study progression Presented at the 31st EADV Congress. Matthews, Ian, et al. "Muscle-specific receptor tyrosine kinase autoantibodies—a new immunoprecipitation assay." Clinica chimica acta 348.1-2 (2004): 95-99. McConville, John, et al. "Detection and characterization of MuSK antibodies in seronegative myasthenia gravis." Annals of neurology 55.4 (2004): 580-584. Marino, Mariapaola, et al. "Long-lasting rituximab-induced reduction of specific—but not total—IgG4 in MuSK-positive myasthenia gravis." Frontiers in immunology 11 (2020): 613. Includes five disclosed product candidates and two undisclosed pipeline disease targets in our pipeline. Developing highly specific CAAR T products to treat B cell-mediated autoimmune diseases Cell therapy pipeline6 targeting diseases that affect over 80,000 U.S. patients MusCAARTes™ trial in patients with MuSK myasthenia gravis on track to initiate in 2022 Circulating anti-MuSK antibody titers may be ~90% lower than anti-DSG3 antibody titers in pemphigus vulgaris3,4,5 DesCAARTes™ trial in patients with mucosal pemphigus vulgaris (mPV) ongoing Favorable safety profile for DSG3-CAART with no dose-limiting toxicities (DLTs) in cohorts A1 to A51 DSG3-CAART persistence through day 29 was similar between cohorts A4 and A5 despite a substantial increase in dose2 One cohort A4 subject with sustained persistence had transient improvement in several efficacy assessments at 3 months post-infusion2 Combination sub-study (pre-treatment with IVIg + cyclophosphamide) prioritized to potentially enhance in vivo DSG3-CAART exposure Cash runway through 1Q24 with $96.8M in cash and investments at the end of 2Q22
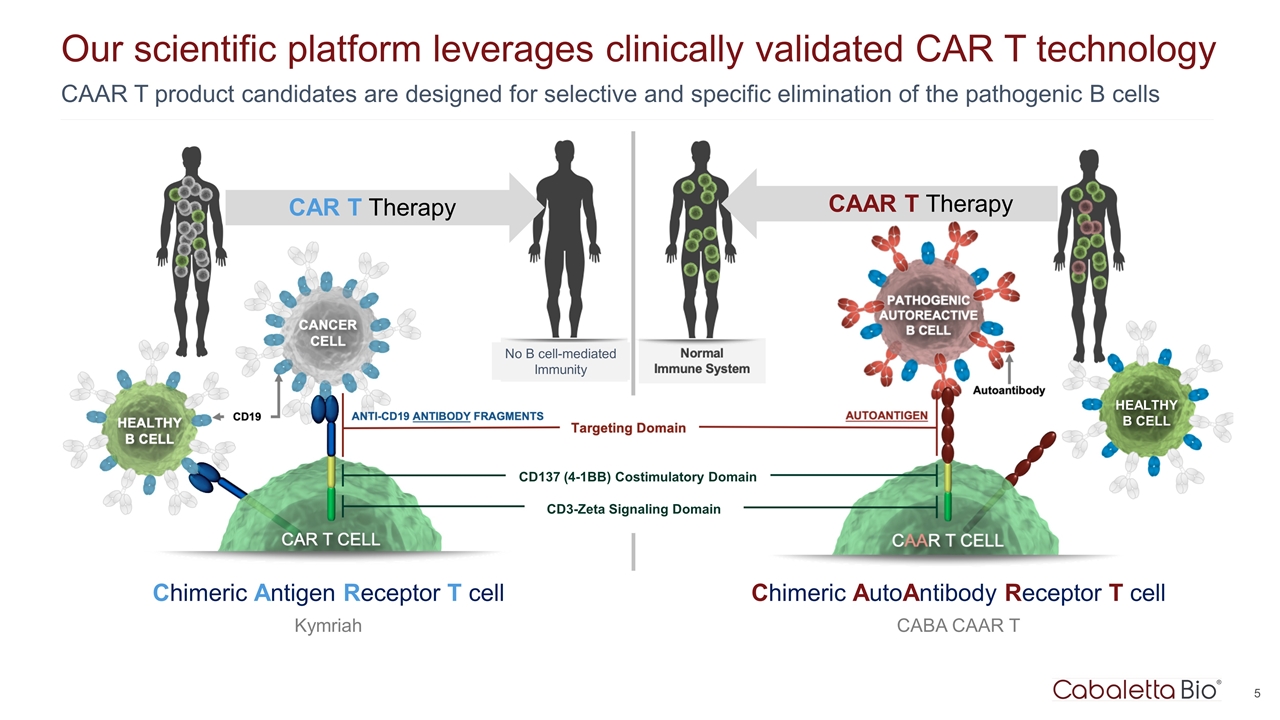
Our scientific platform leverages clinically validated CAR T technology CAR T Therapy Chimeric Antigen Receptor T cell Kymriah CAAR T product candidates are designed for selective and specific elimination of the pathogenic B cells CAAR T Therapy Chimeric AutoAntibody Receptor T cell CABA CAAR T CD137 (4-1BB) Costimulatory Domain CD3-Zeta Signaling Domain HEALTHY B CELL No B cell-mediated Immunity
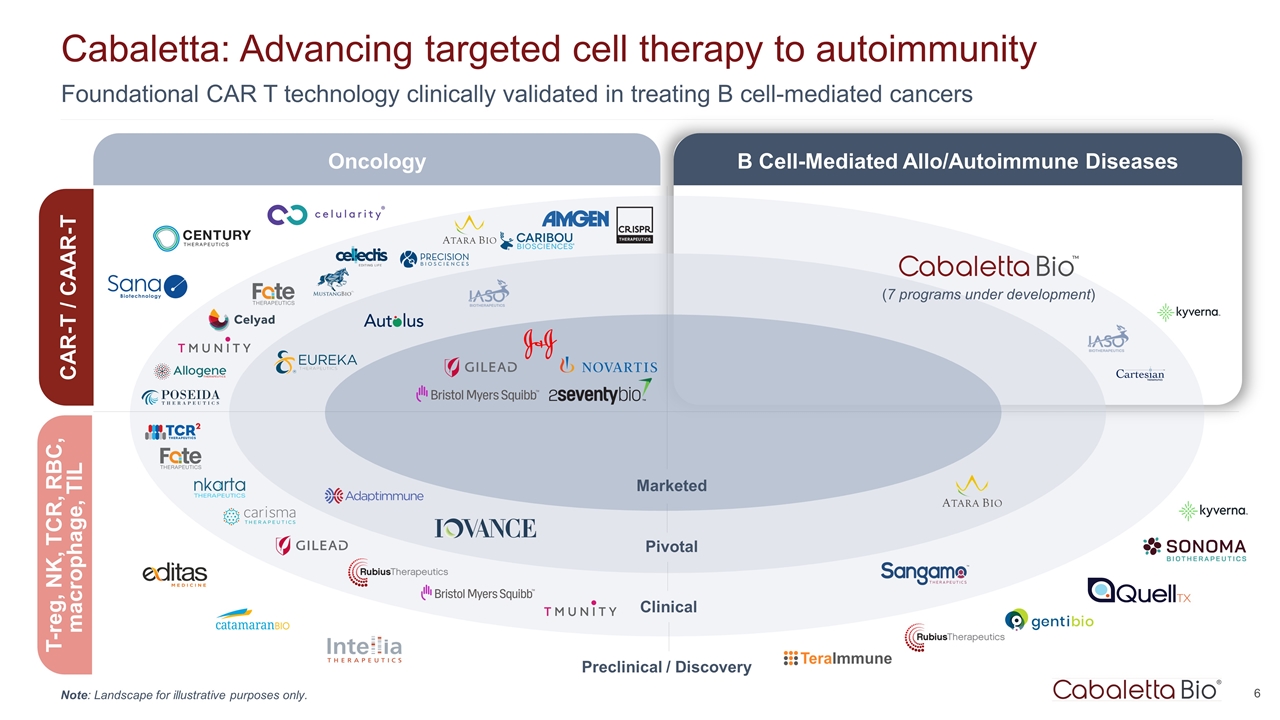
Foundational CAR T technology clinically validated in treating B cell-mediated cancers Cabaletta: Advancing targeted cell therapy to autoimmunity Marketed Pivotal Clinical Preclinical / Discovery Oncology B Cell-Mediated Allo/Autoimmune Diseases CAR-T / CAAR-T T-reg, NK, TCR, RBC, macrophage, TIL (7 programs under development) Note: Landscape for illustrative purposes only.
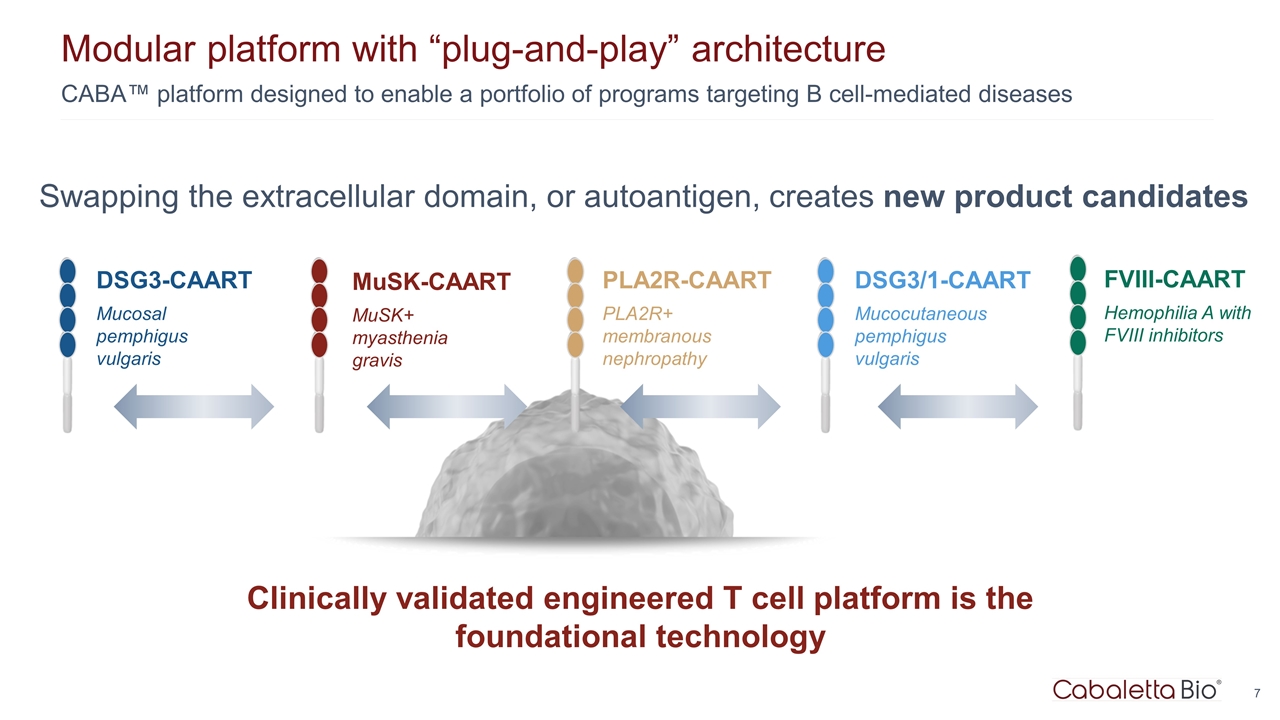
CABA™ platform designed to enable a portfolio of programs targeting B cell-mediated diseases Modular platform with “plug-and-play” architecture Clinically validated engineered T cell platform is the foundational technology PLA2R-CAART PLA2R+ membranous nephropathy DSG3-CAART Mucosal pemphigus vulgaris MuSK-CAART MuSK+ myasthenia gravis DSG3/1-CAART Mucocutaneous pemphigus vulgaris Swapping the extracellular domain, or autoantigen, creates new product candidates FVIII-CAART Hemophilia A with FVIII inhibitors
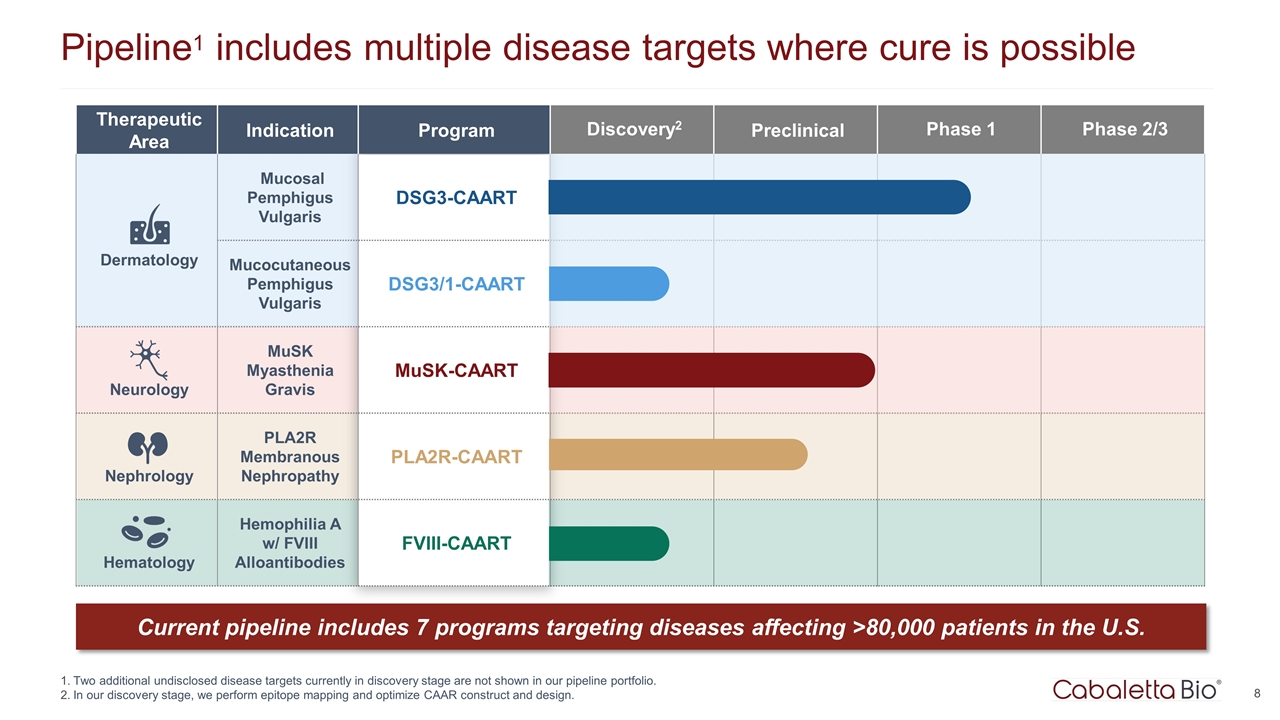
Therapeutic Area Indication Program Discovery2 Preclinical Phase 1 Phase 2/3 Dermatology Mucosal Pemphigus Vulgaris DSG3-CAART Mucocutaneous Pemphigus Vulgaris DSG3/1-CAART Neurology MuSK Myasthenia Gravis MuSK-CAART Nephrology PLA2R Membranous Nephropathy PLA2R-CAART Hematology Hemophilia A w/ FVIII Alloantibodies FVIII-CAART Pipeline1 includes multiple disease targets where cure is possible Two additional undisclosed disease targets currently in discovery stage are not shown in our pipeline portfolio. In our discovery stage, we perform epitope mapping and optimize CAAR construct and design. Current pipeline includes 7 programs targeting diseases affecting >80,000 patients in the U.S.

DSG3-CAART for patients with mucosal pemphigus vulgaris
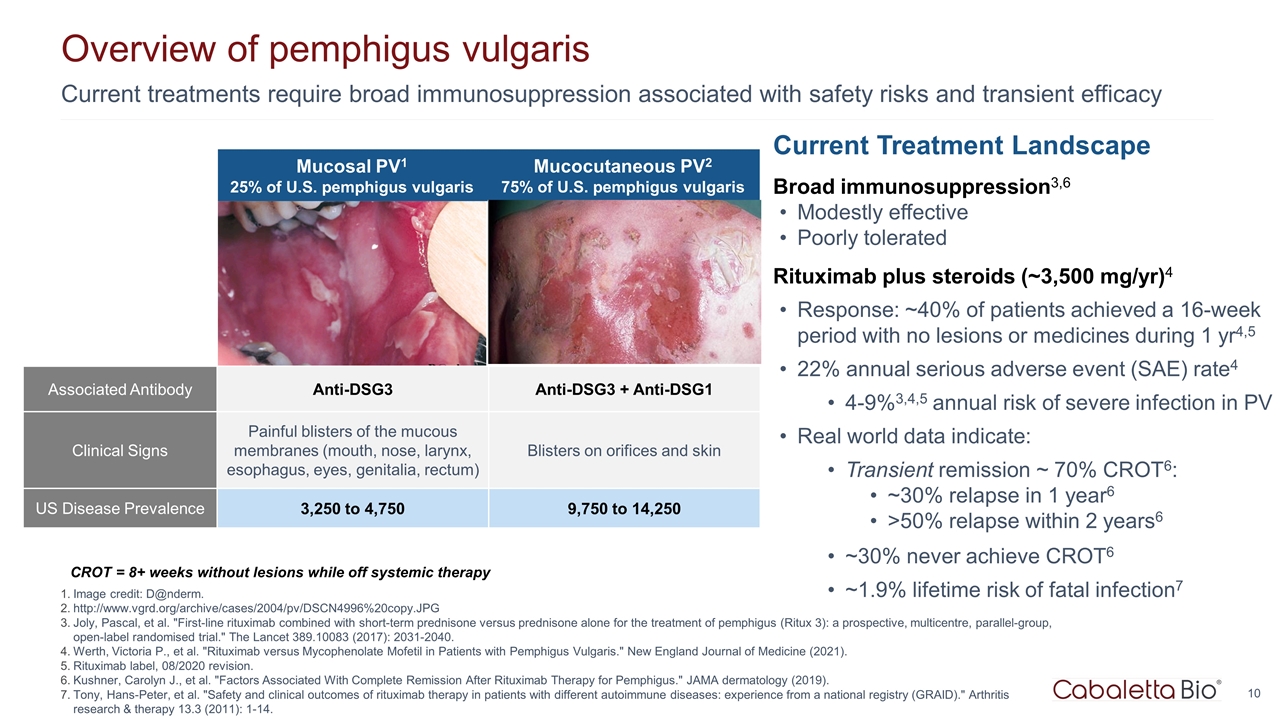
Current treatments require broad immunosuppression associated with safety risks and transient efficacy Overview of pemphigus vulgaris Image credit: D@nderm. http://www.vgrd.org/archive/cases/2004/pv/DSCN4996%20copy.JPG Joly, Pascal, et al. "First-line rituximab combined with short-term prednisone versus prednisone alone for the treatment of pemphigus (Ritux 3): a prospective, multicentre, parallel-group, open-label randomised trial." The Lancet 389.10083 (2017): 2031-2040. Werth, Victoria P., et al. "Rituximab versus Mycophenolate Mofetil in Patients with Pemphigus Vulgaris." New England Journal of Medicine (2021). Rituximab label, 08/2020 revision. Kushner, Carolyn J., et al. "Factors Associated With Complete Remission After Rituximab Therapy for Pemphigus." JAMA dermatology (2019). Tony, Hans-Peter, et al. "Safety and clinical outcomes of rituximab therapy in patients with different autoimmune diseases: experience from a national registry (GRAID)." Arthritis research & therapy 13.3 (2011): 1-14. Current Treatment Landscape Broad immunosuppression3,6 Modestly effective Poorly tolerated Rituximab plus steroids (~3,500 mg/yr)4 Response: ~40% of patients achieved a 16-week period with no lesions or medicines during 1 yr4,5 22% annual serious adverse event (SAE) rate4 4-9%3,4,5 annual risk of severe infection in PV Real world data indicate: Transient remission ~ 70% CROT6: ~30% relapse in 1 year6 >50% relapse within 2 years6 ~30% never achieve CROT6 ~1.9% lifetime risk of fatal infection7 CROT = 8+ weeks without lesions while off systemic therapy http://www.danderm-pdv.is.kkh.dk/atlas/3-157.html http://www.dermis.net/bilder/CD008/550px/img0042.jpg Mucosal PV1 25% of U.S. pemphigus vulgaris Mucocutaneous PV2 75% of U.S. pemphigus vulgaris Associated Antibody Anti-DSG3 Anti-DSG3 + Anti-DSG1 Clinical Signs Painful blisters of the mucous membranes (mouth, nose, larynx, esophagus, eyes, genitalia, rectum) Blisters on orifices and skin US Disease Prevalence 3,250 to 4,750 9,750 to 14,250
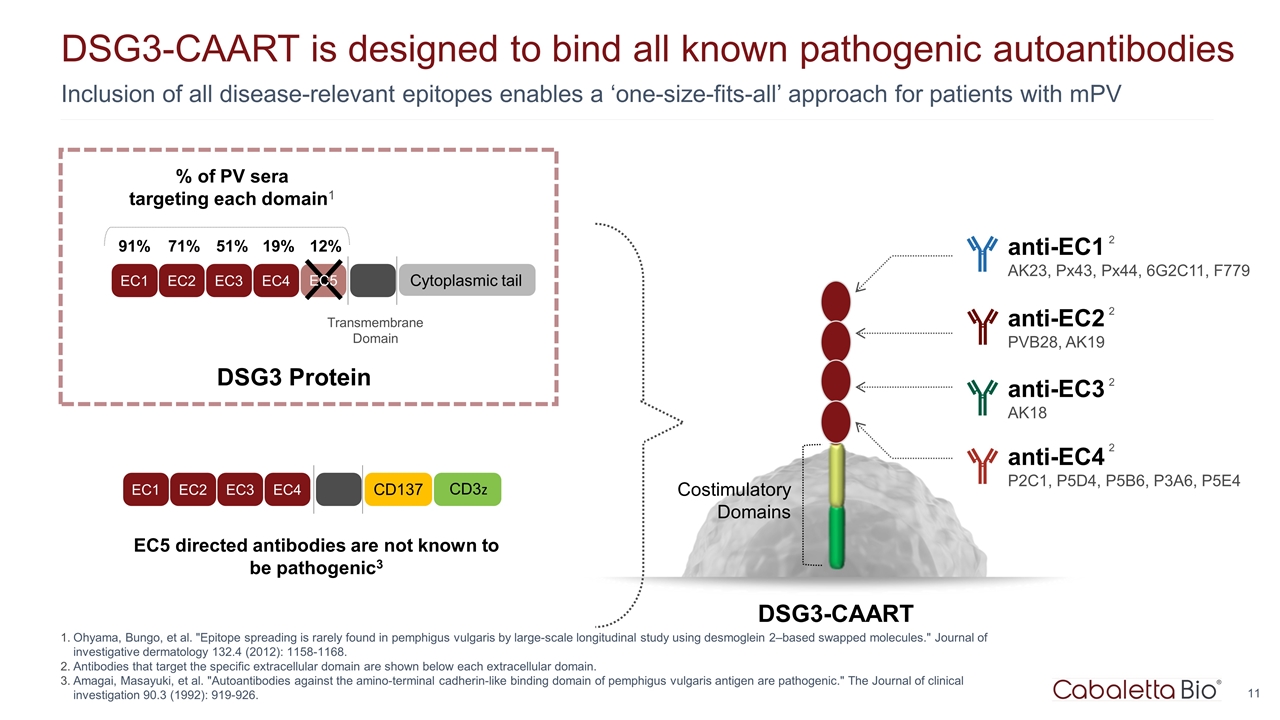
Inclusion of all disease-relevant epitopes enables a ‘one-size-fits-all’ approach for patients with mPV DSG3-CAART is designed to bind all known pathogenic autoantibodies Ohyama, Bungo, et al. "Epitope spreading is rarely found in pemphigus vulgaris by large-scale longitudinal study using desmoglein 2–based swapped molecules." Journal of investigative dermatology 132.4 (2012): 1158-1168. Antibodies that target the specific extracellular domain are shown below each extracellular domain. Amagai, Masayuki, et al. "Autoantibodies against the amino-terminal cadherin-like binding domain of pemphigus vulgaris antigen are pathogenic." The Journal of clinical investigation 90.3 (1992): 919-926. EC5 directed antibodies are not known to be pathogenic3 DSG3-CAART Costimulatory Domains anti-EC4 P2C1, P5D4, P5B6, P3A6, P5E4 2 anti-EC3 AK18 2 anti-EC2 PVB28, AK19 2 anti-EC1 AK23, Px43, Px44, 6G2C11, F779 2 EC1 EC2 EC3 EC4 Transmembrane Domain Cytoplasmic tail % of PV sera targeting each domain1 91% 71% 51% 19% 12% EC5 EC1 EC2 EC3 EC4 CD137 CD3z DSG3 Protein
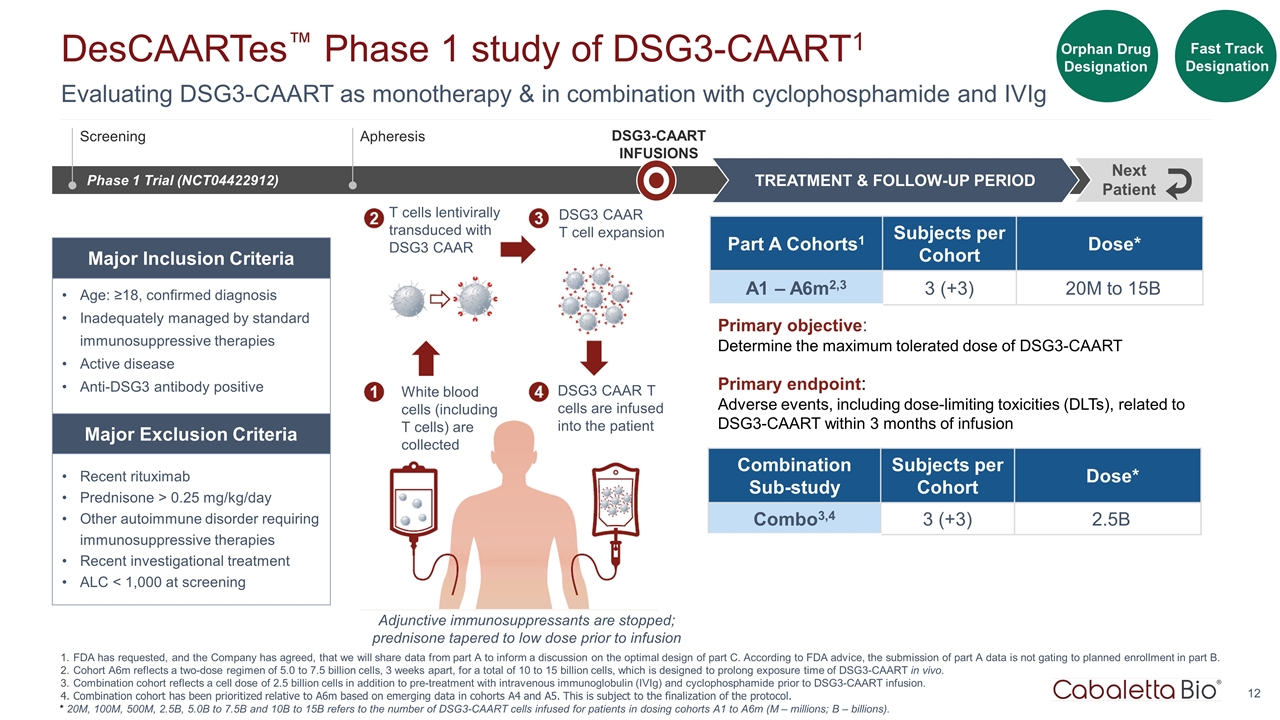
White blood cells (including T cells) are collected T cells lentivirally transduced with DSG3 CAAR DSG3 CAAR T cell expansion DSG3 CAAR T cells are infused into the patient Adjunctive immunosuppressants are stopped; prednisone tapered to low dose prior to infusion Evaluating DSG3-CAART as monotherapy & in combination with cyclophosphamide and IVIg DesCAARTes™ Phase 1 study of DSG3-CAART1 FDA has requested, and the Company has agreed, that we will share data from part A to inform a discussion on the optimal design of part C. According to FDA advice, the submission of part A data is not gating to planned enrollment in part B. Cohort A6m reflects a two-dose regimen of 5.0 to 7.5 billion cells, 3 weeks apart, for a total of 10 to 15 billion cells, which is designed to prolong exposure time of DSG3-CAART in vivo. Combination cohort reflects a cell dose of 2.5 billion cells in addition to pre-treatment with intravenous immunoglobulin (IVIg) and cyclophosphamide prior to DSG3-CAART infusion. Combination cohort has been prioritized relative to A6m based on emerging data in cohorts A4 and A5. This is subject to the finalization of the protocol. Orphan Drug Designation Fast Track Designation Phase 1 Trial (NCT04422912) DSG3-CAART INFUSIONS TREATMENT & FOLLOW-UP PERIOD Next Patient Part A Cohorts1 Subjects per Cohort Dose* A1 – A6m2,3 3 (+3) 20M to 15B Age: ≥18, confirmed diagnosis Inadequately managed by standard immunosuppressive therapies Active disease Anti-DSG3 antibody positive Recent rituximab Prednisone > 0.25 mg/kg/day Other autoimmune disorder requiring immunosuppressive therapies Recent investigational treatment ALC < 1,000 at screening Major Inclusion Criteria Major Exclusion Criteria Screening Apheresis Primary objective: Determine the maximum tolerated dose of DSG3-CAART Primary endpoint: Adverse events, including dose-limiting toxicities (DLTs), related to DSG3-CAART within 3 months of infusion * 20M, 100M, 500M, 2.5B, 5.0B to 7.5B and 10B to 15B refers to the number of DSG3-CAART cells infused for patients in dosing cohorts A1 to A6m (M – millions; B – billions). Combination Sub-study Subjects per Cohort Dose* Combo3,4 3 (+3) 2.5B
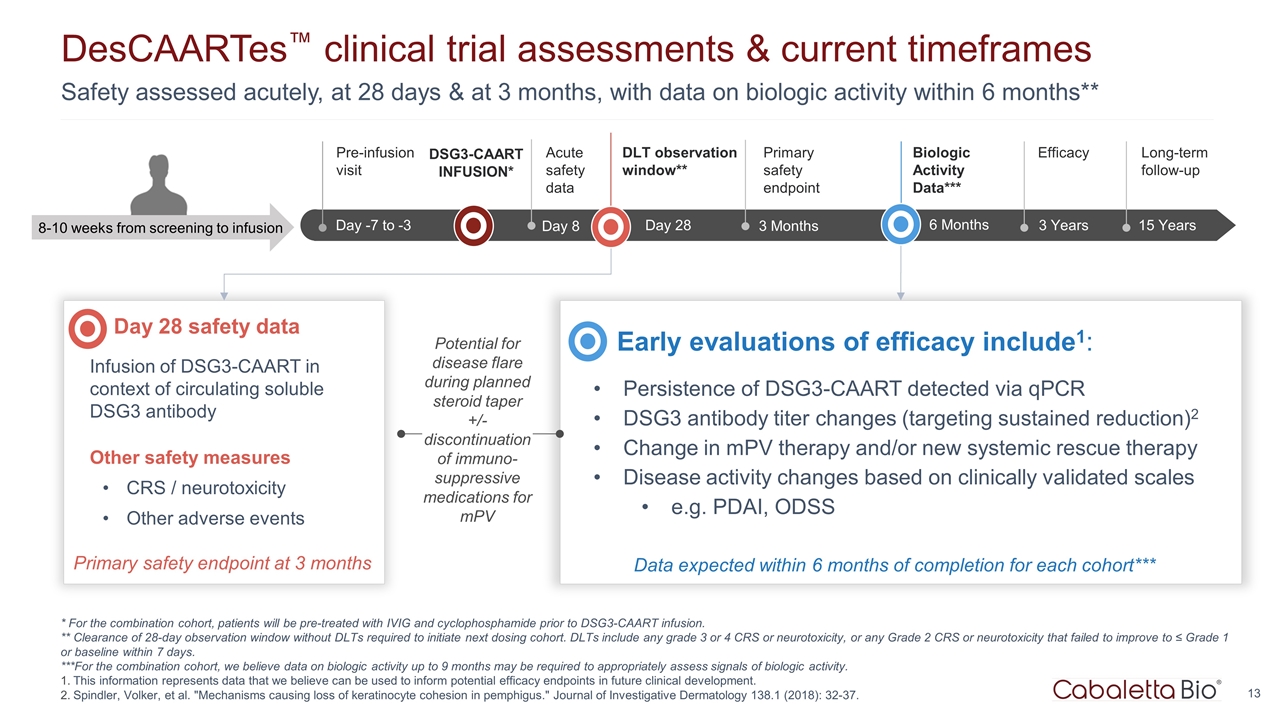
Safety assessed acutely, at 28 days & at 3 months, with data on biologic activity within 6 months** DesCAARTes™ clinical trial assessments & current timeframes * For the combination cohort, patients will be pre-treated with IVIG and cyclophosphamide prior to DSG3-CAART infusion. ** Clearance of 28-day observation window without DLTs required to initiate next dosing cohort. DLTs include any grade 3 or 4 CRS or neurotoxicity, or any Grade 2 CRS or neurotoxicity that failed to improve to ≤ Grade 1 or baseline within 7 days. ***For the combination cohort, we believe data on biologic activity up to 9 months may be required to appropriately assess signals of biologic activity. This information represents data that we believe can be used to inform potential efficacy endpoints in future clinical development. Spindler, Volker, et al. "Mechanisms causing loss of keratinocyte cohesion in pemphigus." Journal of Investigative Dermatology 138.1 (2018): 32-37. Up to Wk -18 Wk -18 to -1 Day -7 to -3 Pre-infusion visit 3 Years Efficacy 15 Years Long-term follow-up 3 Months Primary safety endpoint 8-10 weeks from screening to infusion DSG3-CAART INFUSION* Day 28 safety data Infusion of DSG3-CAART in context of circulating soluble DSG3 antibody Other safety measures CRS / neurotoxicity Other adverse events Early evaluations of efficacy include1: Persistence of DSG3-CAART detected via qPCR DSG3 antibody titer changes (targeting sustained reduction)2 Change in mPV therapy and/or new systemic rescue therapy Disease activity changes based on clinically validated scales e.g. PDAI, ODSS Primary safety endpoint at 3 months Potential for disease flare during planned steroid taper +/- discontinuation of immuno-suppressive medications for mPV DLT observation window** 6 Months Biologic Activity Data*** Data expected within 6 months of completion for each cohort*** Day 28 Day 8 Acute safety data
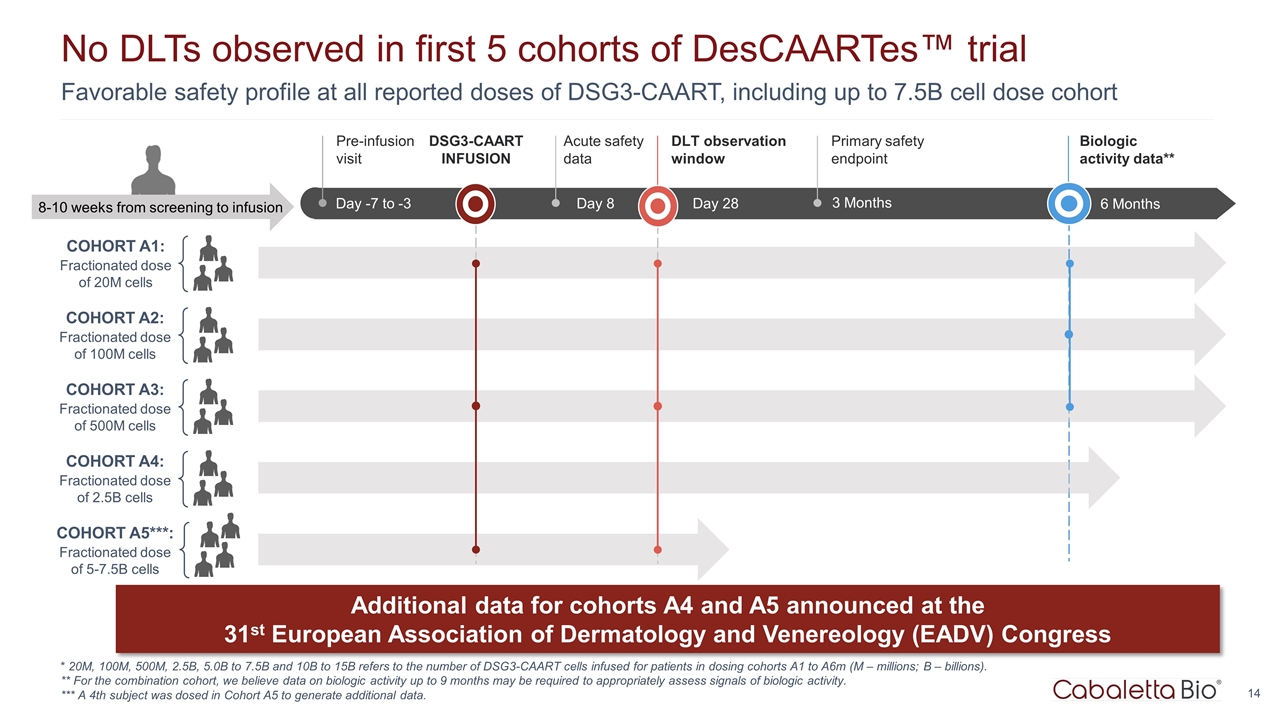
Favorable safety profile at all reported doses of DSG3-CAART, including up to 7.5B cell dose cohort No DLTs observed in first 5 cohorts of DesCAARTes™ trial * 20M, 100M, 500M, 2.5B, 5.0B to 7.5B and 10B to 15B refers to the number of DSG3-CAART cells infused for patients in dosing cohorts A1 to A6m (M – millions; B – billions). ** For the combination cohort, we believe data on biologic activity up to 9 months may be required to appropriately assess signals of biologic activity. *** A 4th subject was dosed in Cohort A5 to generate additional data. COHORT A1: Fractionated dose of 20M cells Up to Wk -18 Wk -18 to -1 Day -7 to -3 Pre-infusion visit Day 8 Acute safety data 8-10 weeks from screening to infusion DSG3-CAART INFUSION Day 28 DLT observation window 3 Months Primary safety endpoint 6 Months Biologic activity data** COHORT A2: Fractionated dose of 100M cells COHORT A3: Fractionated dose of 500M cells COHORT A4: Fractionated dose of 2.5B cells Additional data for cohorts A4 and A5 announced at the 31st European Association of Dermatology and Venereology (EADV) Congress COHORT A5***: Fractionated dose of 5-7.5B cells
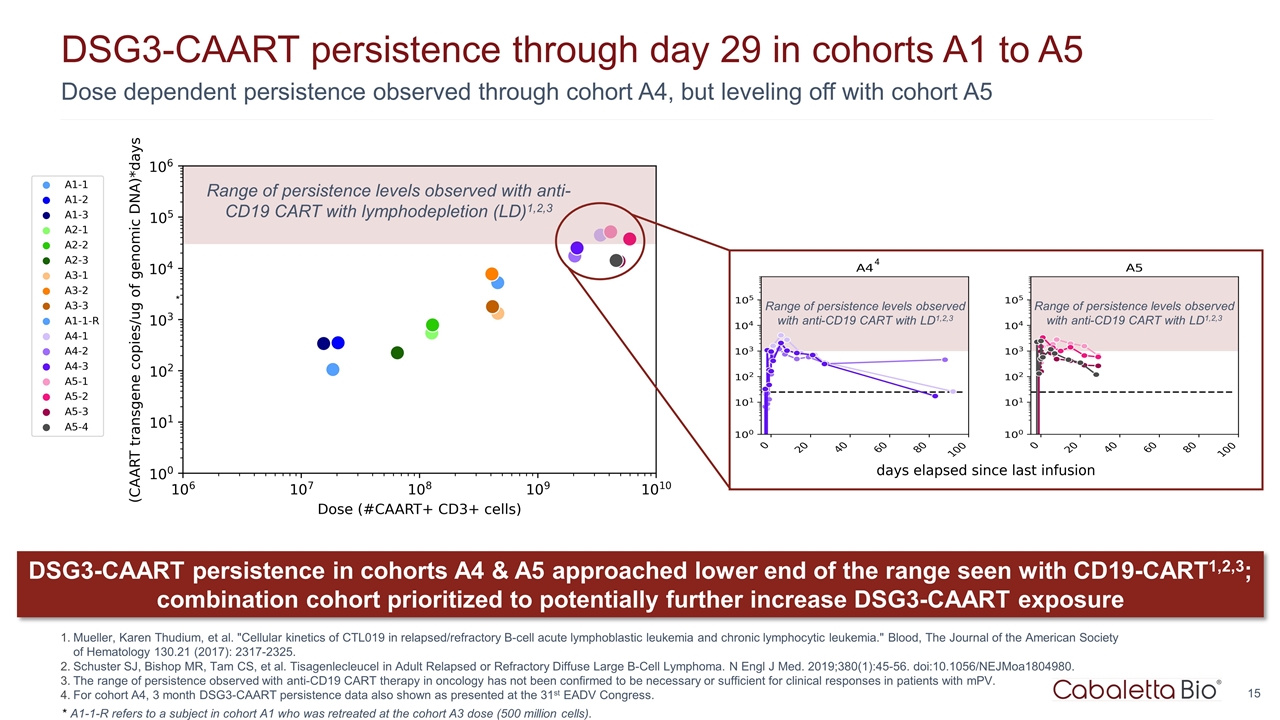
Dose dependent persistence observed through cohort A4, but leveling off with cohort A5 DSG3-CAART persistence through day 29 in cohorts A1 to A5 Mueller, Karen Thudium, et al. "Cellular kinetics of CTL019 in relapsed/refractory B-cell acute lymphoblastic leukemia and chronic lymphocytic leukemia." Blood, The Journal of the American Society of Hematology 130.21 (2017): 2317-2325. Schuster SJ, Bishop MR, Tam CS, et al. Tisagenlecleucel in Adult Relapsed or Refractory Diffuse Large B-Cell Lymphoma. N Engl J Med. 2019;380(1):45-56. doi:10.1056/NEJMoa1804980. The range of persistence observed with anti-CD19 CART therapy in oncology has not been confirmed to be necessary or sufficient for clinical responses in patients with mPV. For cohort A4, 3 month DSG3-CAART persistence data also shown as presented at the 31st EADV Congress. Range of persistence levels observed with anti-CD19 CART with lymphodepletion (LD)1,2,3 Range of persistence levels observed with anti-CD19 CART with LD1,2,3 DSG3-CAART persistence in cohorts A4 & A5 approached lower end of the range seen with CD19-CART1,2,3; combination cohort prioritized to potentially further increase DSG3-CAART exposure * A1-1-R refers to a subject in cohort A1 who was retreated at the cohort A3 dose (500 million cells). * Range of persistence levels observed with anti-CD19 CART with LD1,2,3 4
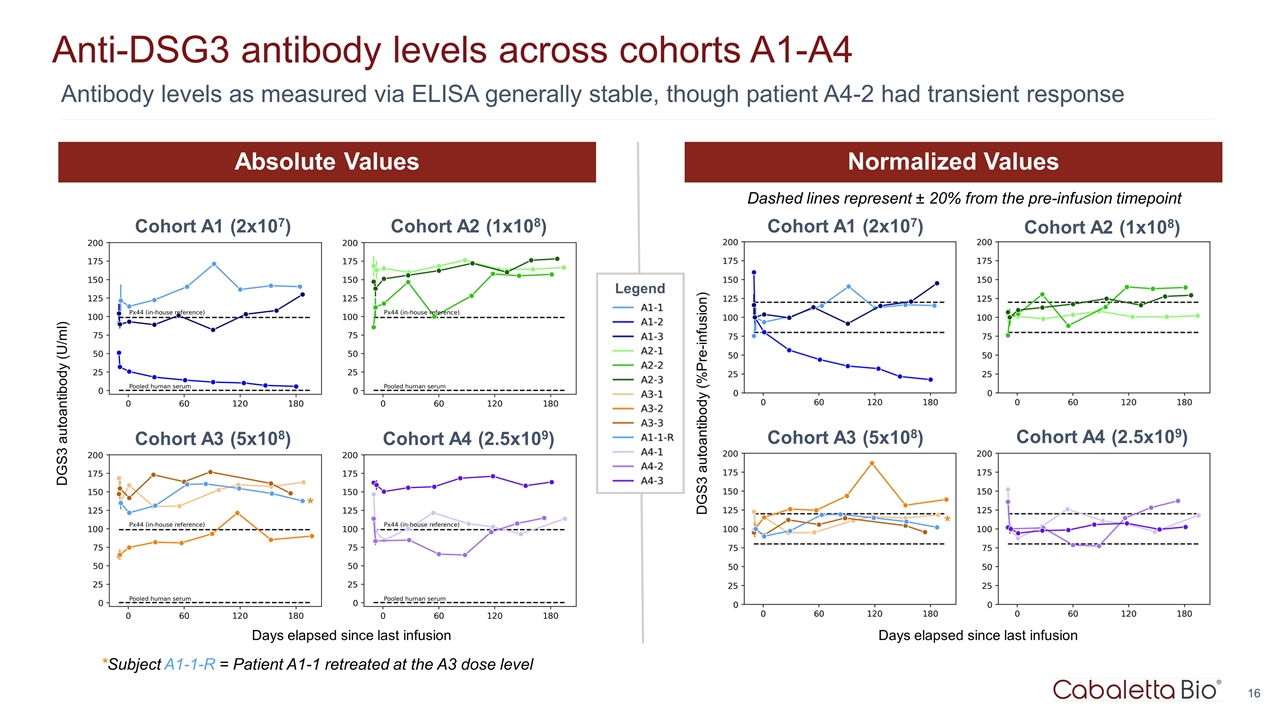
Anti-DSG3 antibody levels across cohorts A1-A4 Antibody levels as measured via ELISA generally stable, though patient A4-2 had transient response Cohort A1 (2x107) Cohort A2 (1x108) Cohort A3 (5x108) Cohort A4 (2.5x109) Cohort A1 (2x107) Cohort A2 (1x108) Cohort A3 (5x108) Cohort A4 (2.5x109) * * Dashed lines represent ± 20% from the pre-infusion timepoint *Subject A1-1-R = Patient A1-1 retreated at the A3 dose level Days elapsed since last infusion Days elapsed since last infusion DGS3 autoantibody (U/ml) Absolute Values Normalized Values DGS3 autoantibody (%Pre-infusion) Legend
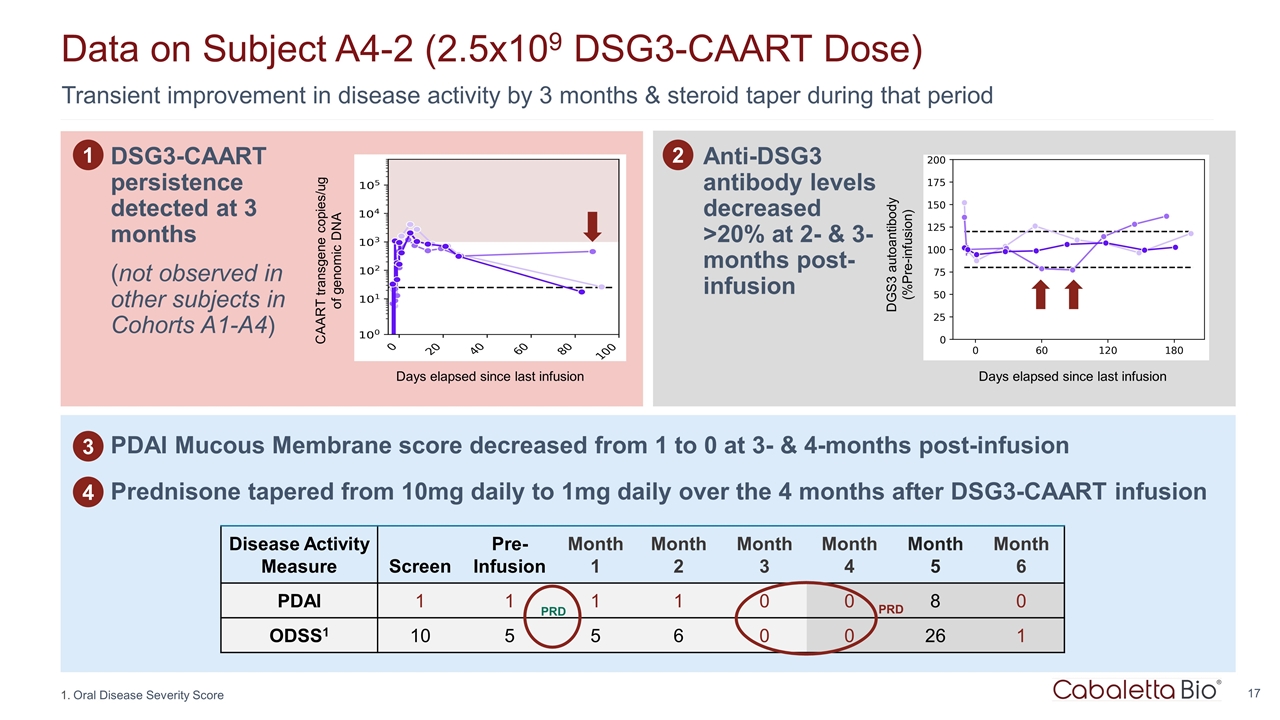
Transient improvement in disease activity by 3 months & steroid taper during that period Data on Subject A4-2 (2.5x109 DSG3-CAART Dose) Oral Disease Severity Score 1 DSG3-CAART persistence detected at 3 months (not observed in other subjects in Cohorts A1-A4) Anti-DSG3 antibody levels decreased >20% at 2- & 3-months post-infusion 2 Disease Activity Measure Screen Pre- Infusion Month 1 Month 2 Month 3 Month 4 Month 5 Month 6 PDAI 1 1 1 1 0 0 8 0 ODSS1 10 5 5 6 0 0 26 1 PRD PRD PDAI Mucous Membrane score decreased from 1 to 0 at 3- & 4-months post-infusion Prednisone tapered from 10mg daily to 1mg daily over the 4 months after DSG3-CAART infusion Days elapsed since last infusion CAART transgene copies/ug of genomic DNA Days elapsed since last infusion DGS3 autoantibody (%Pre-infusion) 3 4
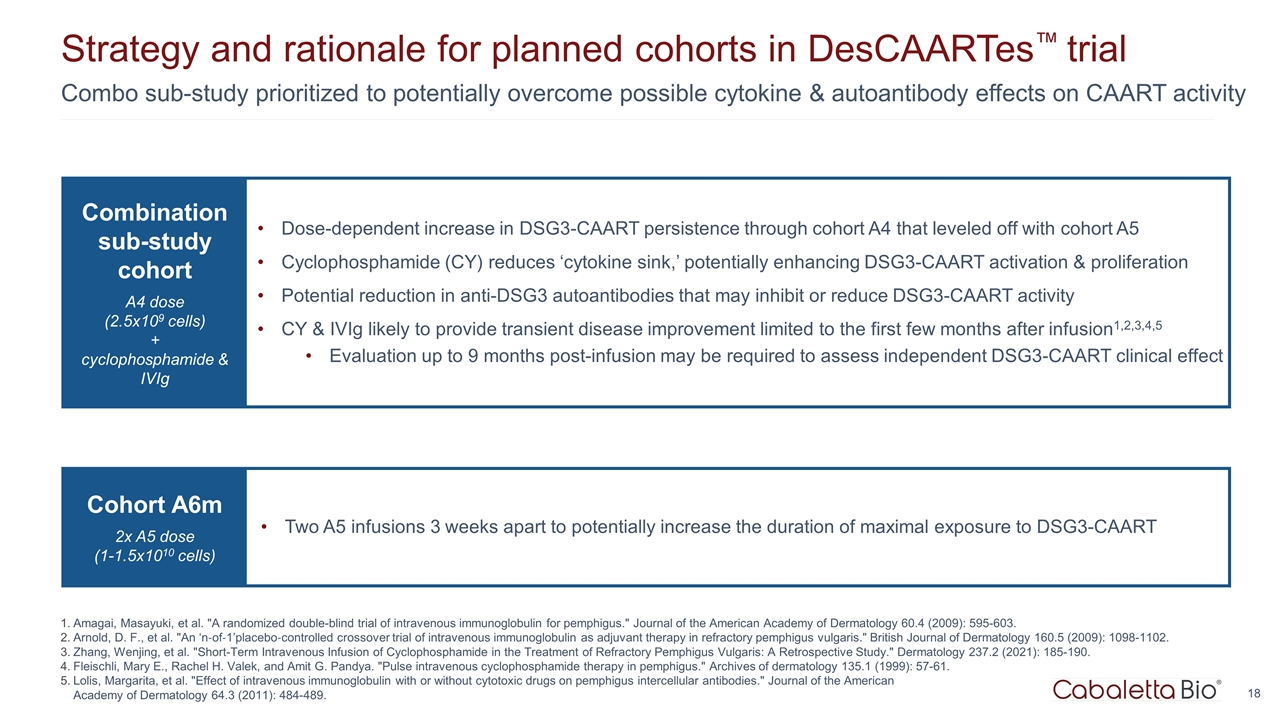
Combo sub-study prioritized to potentially overcome possible cytokine & autoantibody effects on CAART activity Strategy and rationale for planned cohorts in DesCAARTes™ trial Amagai, Masayuki, et al. "A randomized double-blind trial of intravenous immunoglobulin for pemphigus." Journal of the American Academy of Dermatology 60.4 (2009): 595-603. Arnold, D. F., et al. "An ‘n‐of‐1’placebo‐controlled crossover trial of intravenous immunoglobulin as adjuvant therapy in refractory pemphigus vulgaris." British Journal of Dermatology 160.5 (2009): 1098-1102. Zhang, Wenjing, et al. "Short-Term Intravenous Infusion of Cyclophosphamide in the Treatment of Refractory Pemphigus Vulgaris: A Retrospective Study." Dermatology 237.2 (2021): 185-190. Fleischli, Mary E., Rachel H. Valek, and Amit G. Pandya. "Pulse intravenous cyclophosphamide therapy in pemphigus." Archives of dermatology 135.1 (1999): 57-61. Lolis, Margarita, et al. "Effect of intravenous immunoglobulin with or without cytotoxic drugs on pemphigus intercellular antibodies." Journal of the American Academy of Dermatology 64.3 (2011): 484-489. Combination sub-study cohort A4 dose (2.5x109 cells) + cyclophosphamide & IVIg Dose-dependent increase in DSG3-CAART persistence through cohort A4 that leveled off with cohort A5 Cyclophosphamide (CY) reduces ‘cytokine sink,’ potentially enhancing DSG3-CAART activation & proliferation Potential reduction in anti-DSG3 autoantibodies that may inhibit or reduce DSG3-CAART activity CY & IVIg likely to provide transient disease improvement limited to the first few months after infusion1,2,3,4,5 Evaluation up to 9 months post-infusion may be required to assess independent DSG3-CAART clinical effect Cohort A6m 2x A5 dose (1-1.5x1010 cells) Two A5 infusions 3 weeks apart to potentially increase the duration of maximal exposure to DSG3-CAART
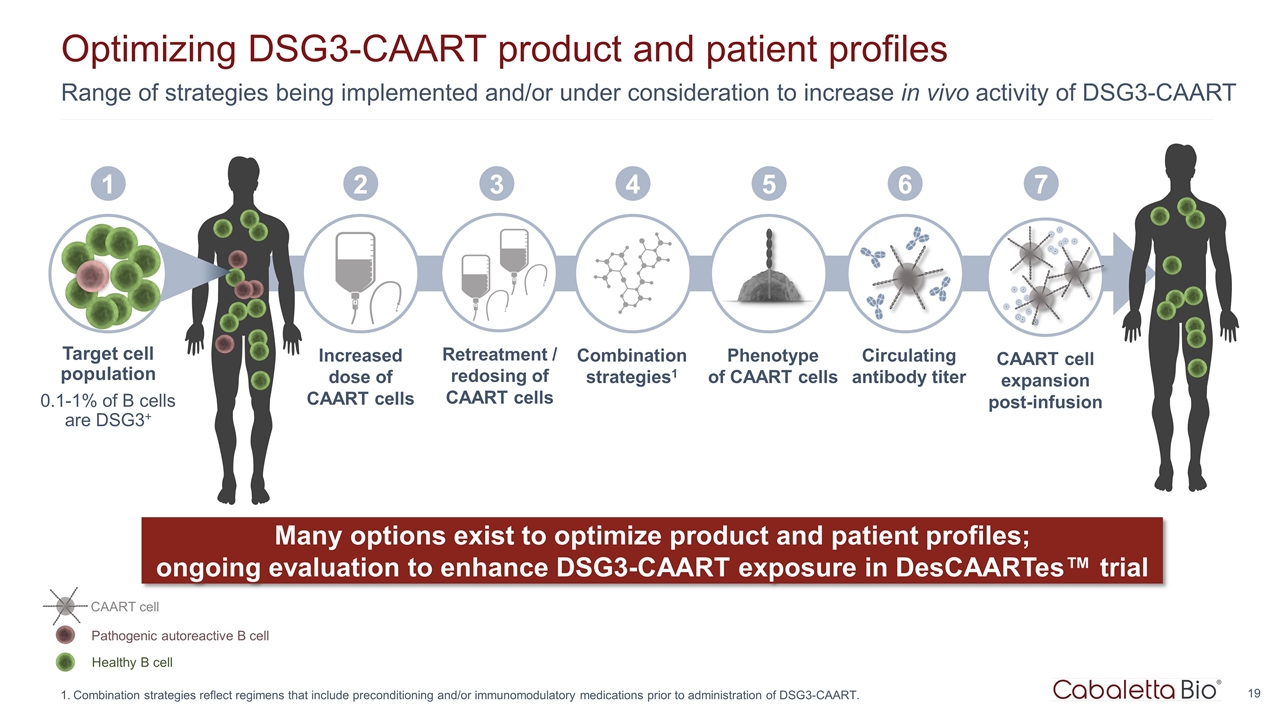
Range of strategies being implemented and/or under consideration to increase in vivo activity of DSG3-CAART Optimizing DSG3-CAART product and patient profiles Many options exist to optimize product and patient profiles; ongoing evaluation to enhance DSG3-CAART exposure in DesCAARTes™ trial Healthy B cell Pathogenic autoreactive B cell CAART cell Increased dose of CAART cells 2 CAART cell expansion post-infusion 3 Target cell population 0.1-1% of B cells are DSG3+ 1 Combination strategies1 4 Circulating antibody titer 6 5 Phenotype of CAART cells Retreatment / redosing of CAART cells 7 Combination strategies reflect regimens that include preconditioning and/or immunomodulatory medications prior to administration of DSG3-CAART.

MuSK-CAART for patients with MuSK myasthenia gravis
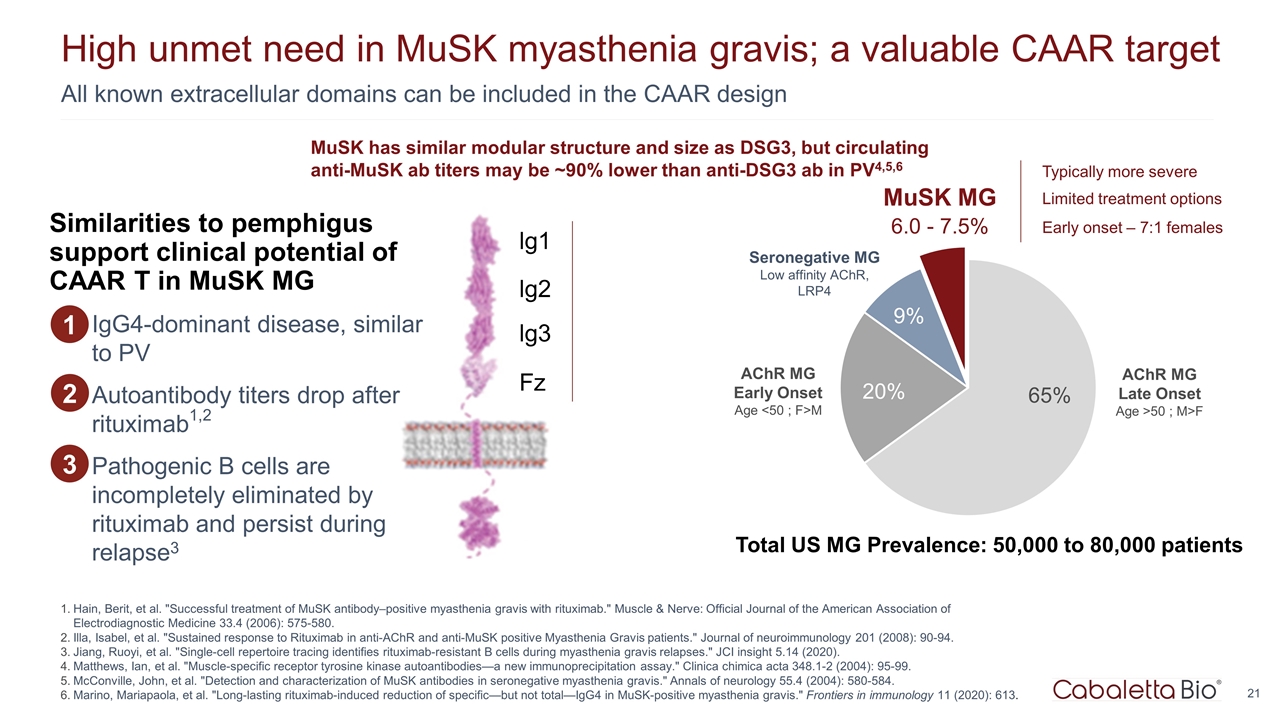
6.0 - 7.5% All known extracellular domains can be included in the CAAR design High unmet need in MuSK myasthenia gravis; a valuable CAAR target Hain, Berit, et al. "Successful treatment of MuSK antibody–positive myasthenia gravis with rituximab." Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine 33.4 (2006): 575-580. Illa, Isabel, et al. "Sustained response to Rituximab in anti-AChR and anti-MuSK positive Myasthenia Gravis patients." Journal of neuroimmunology 201 (2008): 90-94. Jiang, Ruoyi, et al. "Single-cell repertoire tracing identifies rituximab-resistant B cells during myasthenia gravis relapses." JCI insight 5.14 (2020). Matthews, Ian, et al. "Muscle-specific receptor tyrosine kinase autoantibodies—a new immunoprecipitation assay." Clinica chimica acta 348.1-2 (2004): 95-99. McConville, John, et al. "Detection and characterization of MuSK antibodies in seronegative myasthenia gravis." Annals of neurology 55.4 (2004): 580-584. Marino, Mariapaola, et al. "Long-lasting rituximab-induced reduction of specific—but not total—IgG4 in MuSK-positive myasthenia gravis." Frontiers in immunology 11 (2020): 613. AChR MG Early Onset Age <50 ; F>M AChR MG Late Onset Age >50 ; M>F MuSK MG Seronegative MG Low affinity AChR, LRP4 Total US MG Prevalence: 50,000 to 80,000 patients Typically more severe Limited treatment options Early onset – 7:1 females MuSK has similar modular structure and size as DSG3, but circulating anti-MuSK ab titers may be ~90% lower than anti-DSG3 ab in PV4,5,6 lg1 lg2 lg3 Fz IgG4-dominant disease, similar to PV Autoantibody titers drop after rituximab1,2 Pathogenic B cells are incompletely eliminated by rituximab and persist during relapse3 1 Similarities to pemphigus support clinical potential of CAAR T in MuSK MG 2 3
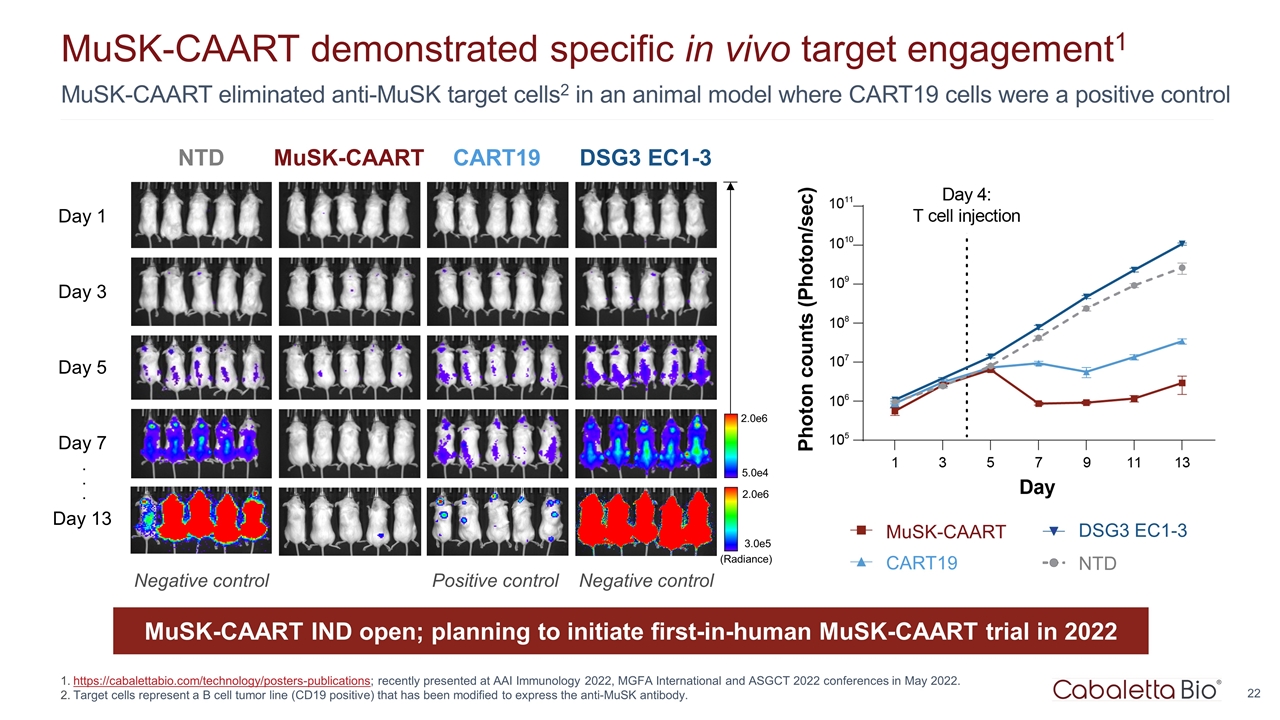
MuSK-CAART eliminated anti-MuSK target cells2 in an animal model where CART19 cells were a positive control MuSK-CAART demonstrated specific in vivo target engagement1 https://cabalettabio.com/technology/posters-publications; recently presented at AAI Immunology 2022, MGFA International and ASGCT 2022 conferences in May 2022. Target cells represent a B cell tumor line (CD19 positive) that has been modified to express the anti-MuSK antibody. MuSK-CAART CART19 DSG3 EC1-3 Day 1 Day 3 Day 5 Day 7 Day 13 5.0e4 2.0e6 (Radiance) 3.0e5 2.0e6 . . . NTD Positive control Negative control Negative control CART19 MuSK-CAART DSG3 EC1-3 NTD MuSK-CAART IND open; planning to initiate first-in-human MuSK-CAART trial in 2022
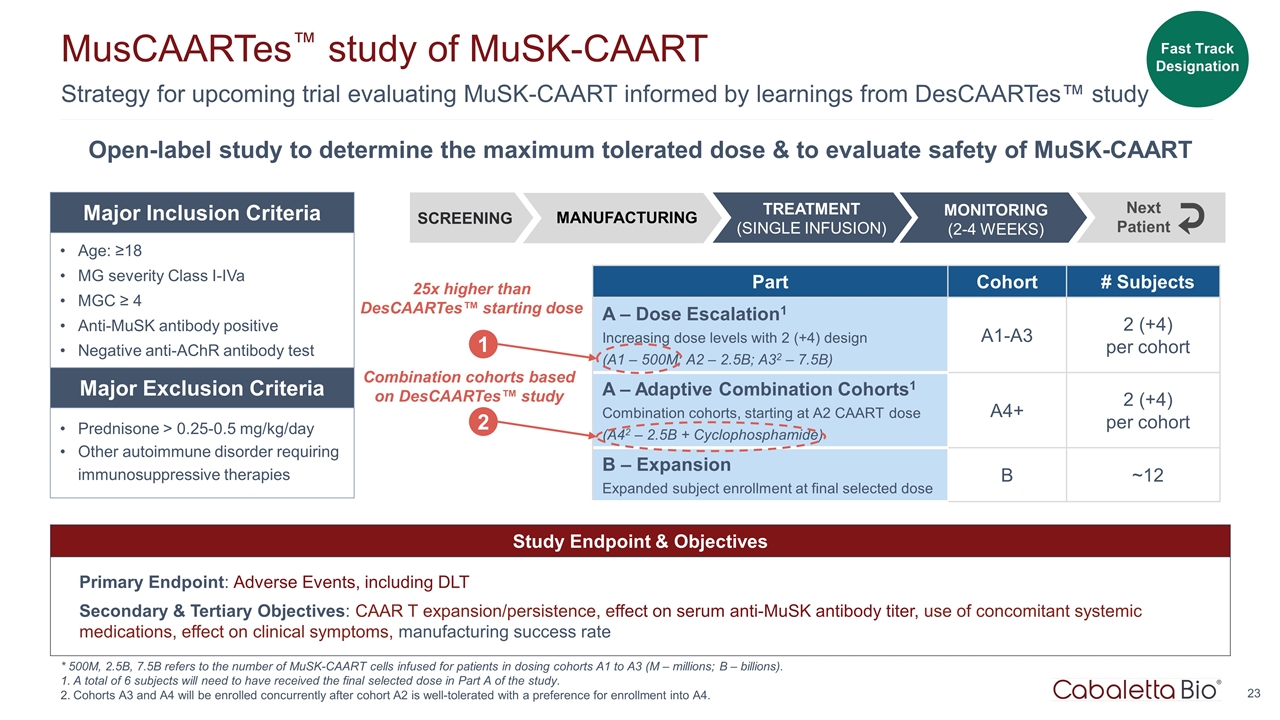
Strategy for upcoming trial evaluating MuSK-CAART informed by learnings from DesCAARTes™ study MusCAARTes™ study of MuSK-CAART * 500M, 2.5B, 7.5B refers to the number of MuSK-CAART cells infused for patients in dosing cohorts A1 to A3 (M – millions; B – billions). A total of 6 subjects will need to have received the final selected dose in Part A of the study. Cohorts A3 and A4 will be enrolled concurrently after cohort A2 is well-tolerated with a preference for enrollment into A4. Study Endpoint & Objectives Primary Endpoint: Adverse Events, including DLT Secondary & Tertiary Objectives: CAAR T expansion/persistence, effect on serum anti-MuSK antibody titer, use of concomitant systemic medications, effect on clinical symptoms, manufacturing success rate Open-label study to determine the maximum tolerated dose & to evaluate safety of MuSK-CAART Part Cohort # Subjects A – Dose Escalation1 Increasing dose levels with 2 (+4) design (A1 – 500M; A2 – 2.5B; A32 – 7.5B) A1-A3 2 (+4) per cohort A – Adaptive Combination Cohorts1 Combination cohorts, starting at A2 CAART dose (A42 – 2.5B + Cyclophosphamide) A4+ 2 (+4) per cohort B – Expansion Expanded subject enrollment at final selected dose B ~12 Age: ≥18 MG severity Class I-IVa MGC ≥ 4 Anti-MuSK antibody positive Negative anti-AChR antibody test Prednisone > 0.25-0.5 mg/kg/day Other autoimmune disorder requiring immunosuppressive therapies Major Inclusion Criteria Major Exclusion Criteria SCREENING MONITORING (2-4 WEEKS) Next Patient MANUFACTURING TREATMENT (SINGLE INFUSION) 1 25x higher than DesCAARTes™ starting dose Fast Track Designation 2 Combination cohorts based on DesCAARTes™ study
PLA2R-CAART for patients with PLA2R-associated membranous nephropathy
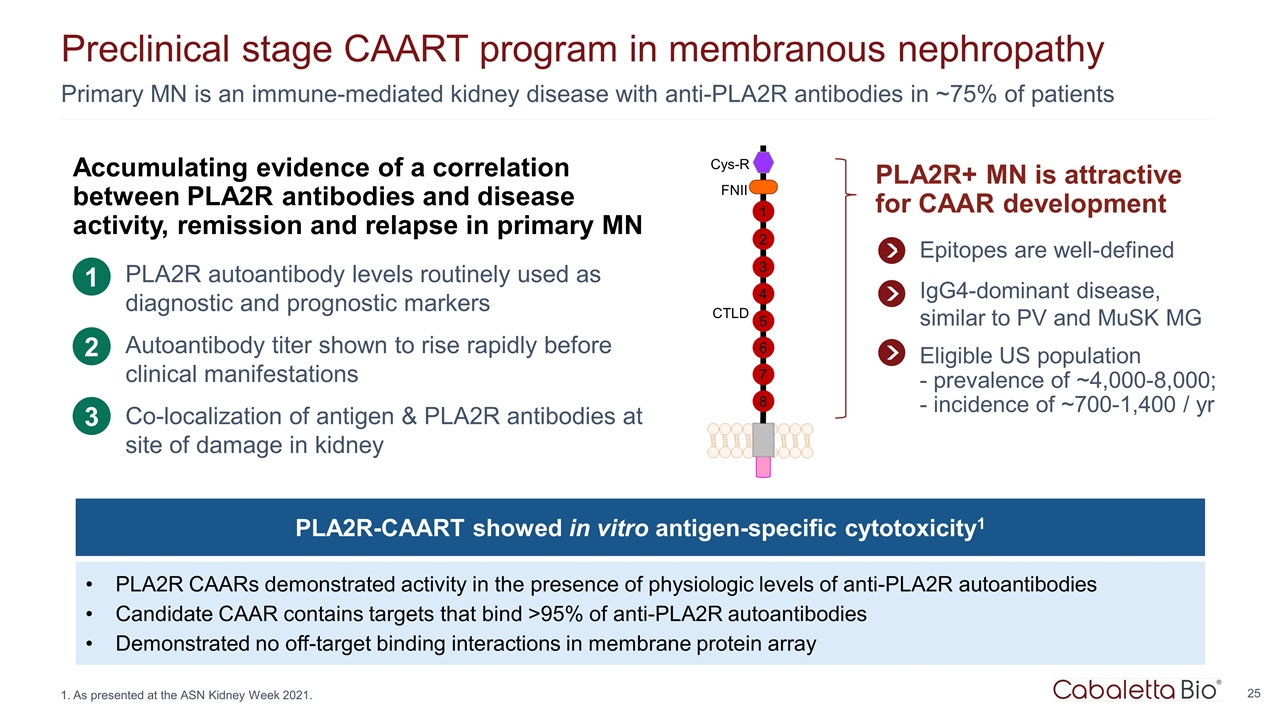
Primary MN is an immune-mediated kidney disease with anti-PLA2R antibodies in ~75% of patients Preclinical stage CAART program in membranous nephropathy Accumulating evidence of a correlation between PLA2R antibodies and disease activity, remission and relapse in primary MN PLA2R autoantibody levels routinely used as diagnostic and prognostic markers Autoantibody titer shown to rise rapidly before clinical manifestations Co-localization of antigen & PLA2R antibodies at site of damage in kidney 1 2 3 Cys-R FNII CTLD 1 2 3 4 5 6 7 8 PLA2R+ MN is attractive for CAAR development Epitopes are well-defined IgG4-dominant disease, similar to PV and MuSK MG Eligible US population - prevalence of ~4,000-8,000; - incidence of ~700-1,400 / yr As presented at the ASN Kidney Week 2021. PLA2R-CAART showed in vitro antigen-specific cytotoxicity1 PLA2R CAARs demonstrated activity in the presence of physiologic levels of anti-PLA2R autoantibodies Candidate CAAR contains targets that bind >95% of anti-PLA2R autoantibodies Demonstrated no off-target binding interactions in membrane protein array
Corporate Summary

BOARD OF DIRECTORS Cabaletta Bio leadership LEADERSHIP TEAM Anup Marda Chief Financial Officer Arun Das, M.D. Chief Business Officer David J. Chang, M.D., M.P.H. Chief Medical Officer Martha O’Connor Chief HR Officer Michael Gerard General Counsel Steven Nichtberger, M.D. President, CEO & Chairman Aimee Payne, M.D., Ph.D. Co-Founder and Co-Chair Michael C. Milone, M.D., Ph.D. Co-Founder and Co-Chair Carl June, M.D. Jay Siegel, M.D. Brian Daniels, M.D. Heather Harte-Hall Chief Compliance Officer Samik Basu, M.D. Chief Scientific Officer Gwendolyn Binder, Ph.D. President, Science & Technology SCIENTIFIC ADVISORY BOARD Steven Nichtberger, M.D. Richard Henriques, M.B.A. Scott Brun, M.D. Mark Simon, M.B.A. Catherine Bollard, M.D. Drew Weissman, M.D., Ph.D. Iain McInnes, Ph.D., FRCP, FRSE, FMedSci
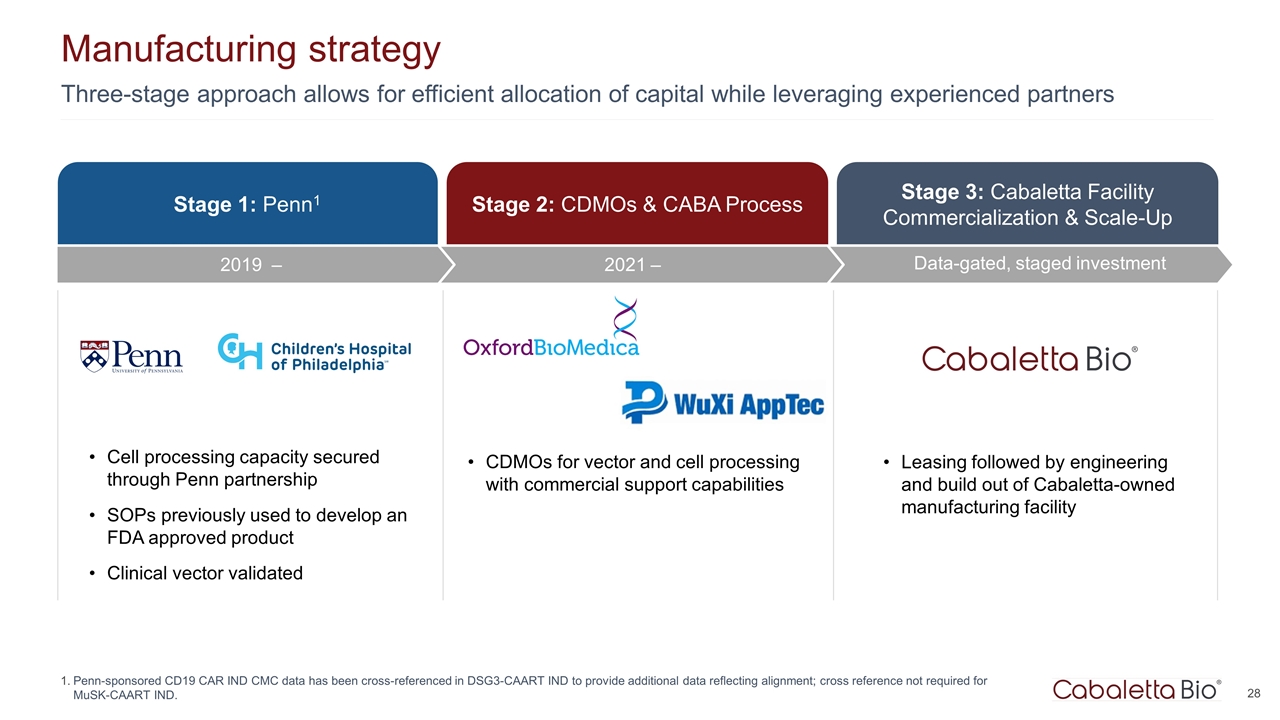
Three-stage approach allows for efficient allocation of capital while leveraging experienced partners Manufacturing strategy Penn-sponsored CD19 CAR IND CMC data has been cross-referenced in DSG3-CAART IND to provide additional data reflecting alignment; cross reference not required for MuSK-CAART IND. Stage 3: Cabaletta Facility Commercialization & Scale-Up Data-gated, staged investment Stage 1: Penn1 Stage 2: CDMOs & CABA Process Cell processing capacity secured through Penn partnership SOPs previously used to develop an FDA approved product Clinical vector validated CDMOs for vector and cell processing with commercial support capabilities Leasing followed by engineering and build out of Cabaletta-owned manufacturing facility 2021 – 2019 –
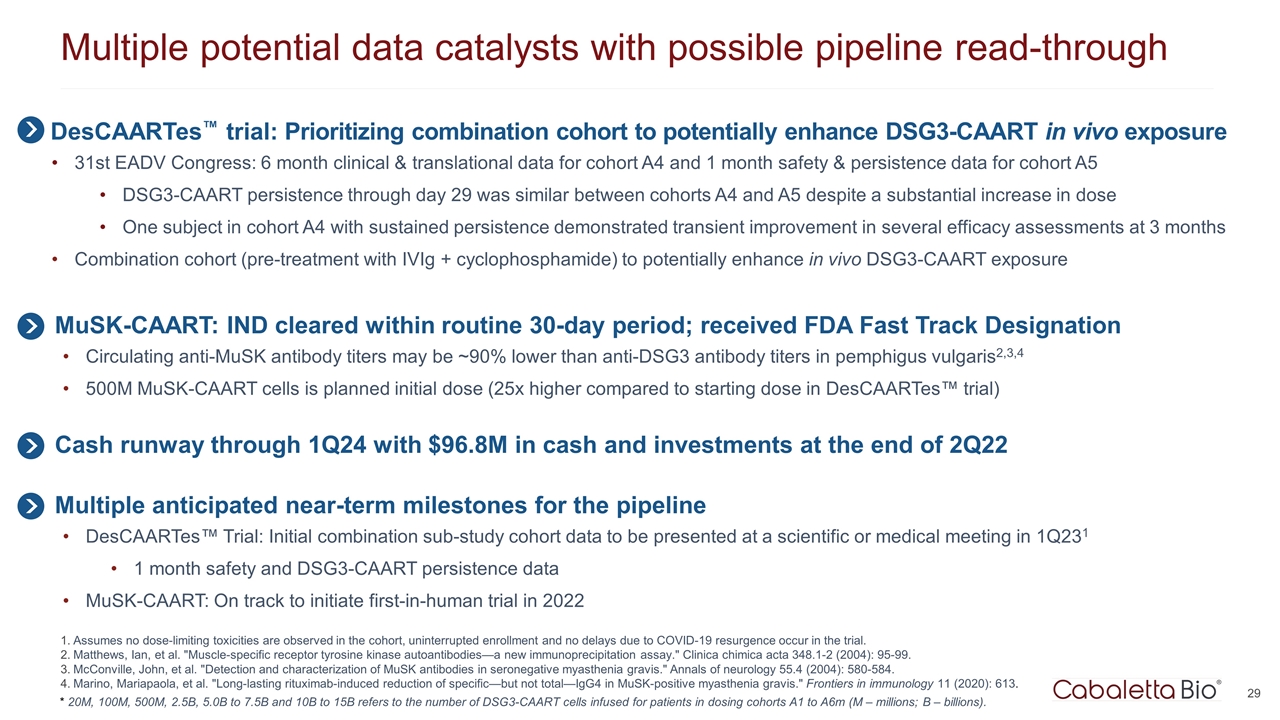
Multiple potential data catalysts with possible pipeline read-through Assumes no dose-limiting toxicities are observed in the cohort, uninterrupted enrollment and no delays due to COVID-19 resurgence occur in the trial. Matthews, Ian, et al. "Muscle-specific receptor tyrosine kinase autoantibodies—a new immunoprecipitation assay." Clinica chimica acta 348.1-2 (2004): 95-99. McConville, John, et al. "Detection and characterization of MuSK antibodies in seronegative myasthenia gravis." Annals of neurology 55.4 (2004): 580-584. Marino, Mariapaola, et al. "Long-lasting rituximab-induced reduction of specific—but not total—IgG4 in MuSK-positive myasthenia gravis." Frontiers in immunology 11 (2020): 613. DesCAARTes™ trial: Prioritizing combination cohort to potentially enhance DSG3-CAART in vivo exposure 31st EADV Congress: 6 month clinical & translational data for cohort A4 and 1 month safety & persistence data for cohort A5 DSG3-CAART persistence through day 29 was similar between cohorts A4 and A5 despite a substantial increase in dose One subject in cohort A4 with sustained persistence demonstrated transient improvement in several efficacy assessments at 3 months Combination cohort (pre-treatment with IVIg + cyclophosphamide) to potentially enhance in vivo DSG3-CAART exposure MuSK-CAART: IND cleared within routine 30-day period; received FDA Fast Track Designation Circulating anti-MuSK antibody titers may be ~90% lower than anti-DSG3 antibody titers in pemphigus vulgaris2,3,4 500M MuSK-CAART cells is planned initial dose (25x higher compared to starting dose in DesCAARTes™ trial) * 20M, 100M, 500M, 2.5B, 5.0B to 7.5B and 10B to 15B refers to the number of DSG3-CAART cells infused for patients in dosing cohorts A1 to A6m (M – millions; B – billions). Cash runway through 1Q24 with $96.8M in cash and investments at the end of 2Q22 Multiple anticipated near-term milestones for the pipeline DesCAARTes™ Trial: Initial combination sub-study cohort data to be presented at a scientific or medical meeting in 1Q231 1 month safety and DSG3-CAART persistence data MuSK-CAART: On track to initiate first-in-human trial in 2022
Corporate Presentation SEPTEMBER 2022